Pig heart transplant recipient dies two months after procedure
Two months following the ground-breaking experiment, the first person to receive the first genetically modified pig heart transplant has died. The patient, 57-year-old David Bennett, passed away on March 8, 2022.
According to the University of Maryland Medical Center (UMMC), where the surgery was performed, Mr. Bennett arrived as a patient with terminal heart disease in October 2021. Hospital staff placed him on a heart-lung bypass machine to keep him alive because his condition was so advanced.
Due to various factors, he was deemed ineligible for a conventional human heart transplant. In cases like this one, the Food and Drug Administration granted emergency authorization for the surgery under “compassionate use” on December 31. Mr. Bennett consented to participate in the novel experimental procedure.
One week later (January 7), doctors performed the surgery and transplanted the pig heart into Mr. Bennett. Four days into recovery, he was taken off the heart-lung machine. According to the UMMC, the transplanted heart performed very well for several weeks without any signs of rejection.
While he convalesced in hospital, he spent time with his family and participated in physical therapy to help build strength. In trying to enjoy the simple pleasures, he watched the Super Bowl with his physical therapist and expressed his desire to return home and reunite with his dog, Lucky.
However, several days ago, his condition began to deteriorate to the point where the medical team acknowledged that he would not recover. He was transferred to compassionate palliative care. In his final hours, he was able to communicate with his family. Doctors did not disclose the exact cause of death.
Dr. Bartley P. Griffith, the transplant surgeon who preformed the surgery said in a statement released by the UMMC: “We are devastated by the loss of Mr. Bennett” and extended sincere condolences to his family.
Interspecies transplant surgeries (known as xenotransplantation) have failed in the past. The failures occur in large part because the transplanted animal tissue/organ is not recognized by the human body and, therefore, is rejected. Researchers agree more work needs to be done on gene-modified animal organs to ascertain the efficacy, viability and long-term outcomes of such procedures.
The medical team at UMMC expressed gratitude for Mr. Bennett’s “unique and historic role in helping contribute to the vast array of knowledge to the field of xenotransplantation”.
Dr. Griffin remains optimistic about the future, adding that this surgery has “led to valuable insights that will hopefully inform transplant surgeons to improve outcomes and potentially lifesaving benefits to future patients”.
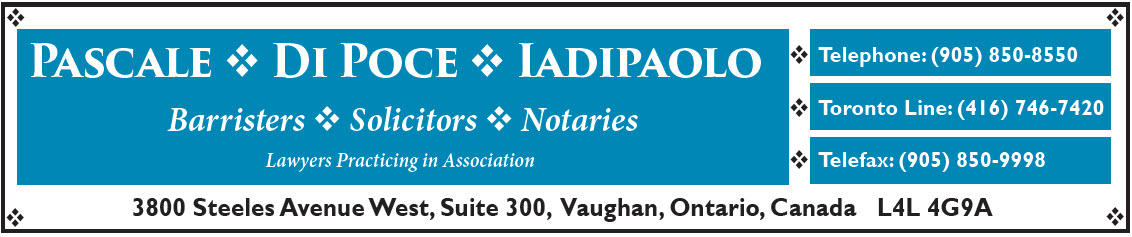
Photo credit: University of Maryland School of Medicine, Dr. Griffin and patient, David Bennett